Will it affect the baby or your labour? Here’s the information you need if you have been told you might have a low-lying placenta or placenta praevia.
What is the role of the placenta anyway?
When you’re pregnant, the placenta develops along with your baby to provide nutrients and oxygen. It attaches to the wall of your uterus, connecting your baby with your blood system. After your baby is born the placenta will come out, which is why it’s also known as the afterbirth (RCOG, 2018a).
What is a low-lying placenta?
When the placenta attaches low in the uterus, you’ll hear people referring to it as a low-lying placenta. They’re usually spotted on your routine 20-week ultrasound.
As the uterus grows upwards, the placenta is likely to move away from the cervix. Your midwife will check for this during an extra scan at 32 weeks (RCOG, 2018a). If that scan finds your placenta is still low lying, you’ll have another scan at 36 weeks (RCOG, 2018a).
At that scan, if the placenta has moved to 2cm or more from the inside of the cervix, then you can choose a vaginal birth (RCOG, 2018a).
If not, it’s defined as placenta praevia or previa. Only one in 10 women who have a low-lying placenta will develop placenta praevia (RCOG, 2018a).
Ok, so what is placenta praevia?
When the placenta covers part or all of the cervix in the last months of pregnancy, it is called placenta praevia. It happens in around one in 200 pregnancies (Sekiguchi et al, 2013).
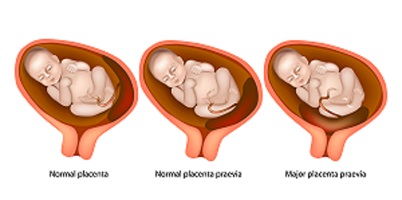
Placenta praevia can be major or minor: a major placenta praevia covers the entire cervix, and a minor placenta praevia covers only a part of it (RCOG, 2018b). You’ll also hear doctors and midwives calling it ‘anterior’ or ‘posterior’ placenta praevia. This depends on whether it is located on the front (anterior) or posterior (back) wall of the uterus (Jang et al, 2011).
What are the risks of placenta praevia?
With placenta praevia, there is a chance of bleeding in the second half of pregnancy. That’s because this is when the placenta lies in the lower part of the womb, which is stretching as your baby grows (RCOG, 2018a).
The stretching puts the connection between the placenta and the wall of the uterus under strain. The bleeding can be heavy and, in rare cases, risky for your baby.
The chance of bleeding is higher if the placenta is on the front wall of the uterus (Jang et al, 2011).
When the placenta is blocking the baby’s way out, you’ll be advised to have a caesarean birth. This will make sure the baby is born safely (RCOG, 2010, 2018a).
There is also a higher chance of the baby being born prematurely (before 37 weeks) and poorly, as a result of placenta praevia (Sekiguchi et al, 2013).
How do you get a diagnosis for placenta praevia?
Your ultrasound scan will usually be able to detect whether you have placenta praevia (Bhinde et al, 2003). But if your ultrasound isn’t clear, an MRI can show whether you’re at a higher risk of it (RCOG, 2018b).
You might also be suspected of having placenta praevia if you have bleeding in the second half of the pregnancy (RCOG, 2018a). The bleeding is not associated with pain and usually occurs after sex.
Occasionally, placenta praevia may be suspected later in pregnancy. This might happen if the baby is in an unusual position, such as bottom first (breech) or lying across the womb (transverse) (RCOG, 2018a).
What treatment will you have if you have placenta praevia?
"Women with placenta praevia have a high chance of premature births and significant bleeding (RCOG, 2018a). So you’ll have your care tailored to what you need (RCOG, 2018b)."
If that’s you and you experience bleeding, contractions or pain, make sure you contact the hospital and go there immediately. Make sure you have someone with you too (RCOG 2018a, 2018b).
What are the causes of placenta praevia?
The chance of having a placenta praevia is greater if you:
- are over 35 years old
- have had fertility treatment, particularly IVF
- have had uterine surgery or have a uterine abnormality like fibroids
- are expecting more than one baby
- have had a previous caesarean birth
- have had a previous abortion
- are smoking during pregnancy
- are using cocaine during pregnancy
- are expecting a boy.
(Faiz and Ananth, 2003; Laughon et al, 2005; RCOG, 2018a)
Is there anything else to consider if I have a placenta praevia?
If you have a confirmed placenta praevia, you will be advised to avoid penetrative sex during pregnancy. That’s particularly the case if you had bleeding after sex (Polomeno, 2000; Read, 2004; Allen and Fountain, 2007). You will also be offered a speculum examination to see the site and amount of bleeding. Eat lots of iron to cut the risk of anaemia (RCOG, 2018a).
This page was last reviewed in May 2018.
Further information
Our support line offers practical and emotional support with feeding your baby and general enquiries for parents, members and volunteers: 0300 330 0700.
We also offer antenatal courses which are a great way to find out more about birth, labour and life with a new baby.
Bhinde A, Prefumo F, Moore J, Hollis B, Thilaganathan B. Placental edge to internal os distance in the late trimester and mode of delivery in placenta praevia. Obstetric Gyanecol. 110(9):860-864. Available from : https://obgyn.onlinelibrary.wiley.com/doi/full/10.1111/j.1471-0528.2003… [Accessed 17th May 2018]
Faiz AS, Ananth CV. (2003) Etiology and risk factors for placenta previa: an overview and meta-analysis of observational studies. J Matern Fetal Neonatal Med. 13(3):175-190. Available from: https://www.ncbi.nlm.nih.gov/pubmed/12820840 [Accessed 17th May 2018]
Jang DG, We JS, Shin JU, Choi YJ, Ko HS, Park Y, Shin JC. (2011) Maternal outcomes according to placental position in placental previa. Int J Med Sci. 8(5):439-444. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3149424/ [Accessed 17th May 2018]
Laughon SK, Wolfe HM, Visco AG. (2005) Prior caesarean and the risk for placenta previa in second-trimester ultrasonography. Obstet Gynecol. 105:962-965. Available from: https://www.ncbi.nlm.nih.gov/pubmed/15863531 [Accessed 17th May 2018]
RCOG. (2010) Caesarean section for placenta praevia. Consent advice no. 12. Available from: https://www.rcog.org.uk/globalassets/documents/guidelines/ca-12-alt_layout-1.pdf [Accessed 17th May 2018]
RCOG. (2018a) Placenta praevia, placenta accreta and vasa praevia. Available from: https://www.rcog.org.uk/globalassets/documents/patients/patient-information-leaflets/pregnancy/pi-placenta-praevia-placenta-accreta-and-vasa-praevia.pdf [Accessed 17th May 2018]
RCOG. (2018b) Placenta praevia, placenta praevia accrete and vasa praevia: diagnosis and management. Green-top guideline no. 27a. Available from: https://obgyn.onlinelibrary.wiley.com/doi/epdf/10.1111/1471-0528.15306 [Accessed 17th May 2018]
Sekiguchi A, Nakai A, Kawabata I, Hayashi M, Takeshita T. (2013) Type and location of placenta previa affect preterm delivery risk related to antepartum haemorrhage. Int J Med Sci. 10(12):1683-1688. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3804794/ [Accessed 17th May 2018]
Polomeno V. (2000) Sex and Pregnancy: A Perinatal educator’s guide. Journal of Perinatal Education. 9(4):15-27. Available from: https://www.ncbi.nlm.nih.gov/pubmed/17273227 [Accessed 17th May 2018]
Read J. (2004) Sexual problems associated with infertility, pregnancy, and ageing. BMJ. 329(7465):559-561. Available from: https://www.ncbi.nlm.nih.gov/pubmed/15345632 [Accessed 17th May 2018]
Allen L, Fountain L. (2007) Addressing sexuality and pregnancy in childbirth education classes. Journal of Perinatal Education. 16(1):32-36. Available from: https://www.ncbi.nlm.nih.gov/pubmed/18408809 [Accessed 17th May 2018]
Further reading
Wing DA, Paul RH, Millar LK. (1996) Management of the symptomatic placenta previa: a randomized, controlled trial of inpatient versus outpatient expectant management. Am J Obstet Gynecol. 175:806–11. Available from: https://www.ncbi.nlm.nih.gov/pubmed/8885726 [Accessed 17th May 2018]



